Are PARP inhibitors safe and effective in men with elevated prostate cancer risk?
Prostate cancer, the primary cancer of the male reproductive system, affects 1 in 9 men during their lifetime1. For male carriers of the BRCA2 gene mutation, the risk is 1 in 3. These cancers range from slow-growing tumors that may need minimal or no treatment, to aggressive forms that require immediate and intensive care. The choice of treatment for prostate cancer depends on various factors, including the stage of the disease, the patient’s age, and overall health.
In 2023, there were three FDA approvals of the PARP inhibitors (PARPi) in prostate cancer. These included niraparib, olaparib and talazoparib, all in various forms of combination therapies with other drugs, for metastatic castration-resistant prostate cancer in patients with BRCA gene mutations. Niraparib and olaparib in combination have also been approved by Health Canada this year.
Therefore, there is no better time to learn how these drugs work, the potential benefits, and the potential drawbacks of PARPi for prostate cancer treatment, particularly for men who carry a BRCA gene mutation.
Background: Prostate Cancer & Treatments
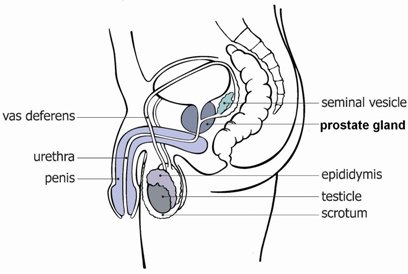
Src: Cancer Council (https://www.cancer.org.au/)
Prostate Cancer: What is it?
Prostate cancer originates in the cells of the prostate. Cancers occur when cells divide uncontrollably caused by changes to DNA. Cancer can spread (metastasize) to other parts of the body and is often life-threatening.
Prostate cancer primarily falls into two categories: castration-sensitive (or hormone-sensitive) and castration-resistant. Castration-resistant prostate cancer is a type of cancer that can progress to metastatic castration-resistant prostate cancer (mCRPC), which is an advanced and terminal condition. mCRPC patients whose disease still progresses after hormone therapy and chemotherapy have a poor prognosis and limited treatment options.
With the new advancements in PARPi, delayed progression and better overall survival are being seen in patients with BRCA mutations with mCRPC. This means that men with mCRPC and who are also known to be BRCA+ can now be offered new options with proven benefits. The value in testing for BRCA genes in men is therefore increasing as these innovative new treatment options become available.
Background: Approaches to Treatment
Treatment for prostate cancer often involves several stages. First-line treatment is a treatment that is accepted as best for the initial treatment of a condition or disease. Second-line treatment is treatment after the initial treatment (first-line treatment) has failed or is no longer working or has side effects that are overly negatively impacting a patient’s quality of life.
Some common first-line treatments for prostate cancer include surgery, hormone therapy, chemotherapy, and/or radiation therapy.
Hormone therapy uses medications to interfere with hormone production or function in the body. These are primarily used in cancers where hormones act as growth factors, such as prostate cancers and other cancers of the reproductive system. Depending on the application of hormone therapy, the drug may affect normal cells that are also sensitive to hormones, which can lead to side effects of muscle loss and bone thinning.
Chemotherapy uses drugs to kill rapidly dividing cancer cells. It's a systemic treatment, meaning it affects the entire body. Chemotherapy can be used as a first-line treatment, before or after surgery, or for advanced cancers.
Radiation therapy uses high-energy particles or waves, like X-rays, gamma rays, electron beams, or protons, to destroy or damage cancer cells. It's often localized to the cancer site (not systemic), however, healthy cells can also be damaged by radiation therapy.
PARP Inhibitors (PARPi)
Why do we need them?
There is a need for new therapies that improve survival in patients with mCRPC (metastatic castration-resistant prostate cancer) who have already gone through two or three lines of treatment or are not medically fit to receive some therapies due to the risk of toxicities.
What are they exactly?
PARPi are a form of targeted therapy, which refers to drugs that target specific genes or proteins that are needed for cancer to grow and survive. They are often more specific and only affect the cancer cells, especially in cancers with specific genetic mutations.
Prolonged survival has been demonstrated with the use of PARPi. In the case of talazoparib, mCRPC patients with the BRCA mutation showed a 77% lower disease progression or death rate when treated compared to those who were not treated. mCRPC patients without the BRCA mutation also showed a 37% lower disease progression or death rate when treated compared to those who were not treated, but the effect is still far more significant in people with BRCA mutations.
Why do they work?
The BRCA1 and BRCA2 genes are very important for repairing DNA damage. BRCA mutations or deficiencies in BRCA genes are commonly present in metastatic prostate cancer: BRCA 1 is present in 7% and BRCA 2 is present in 44% of metastatic prostate cancers.
In cancer cells with deficiencies in the BRCA1 or BRCA2, cells become overly dependent on the PARP protein for DNA repair. This vulnerability is exploited by PARP inhibitors.
PARP inhibitors interfere with the PARP (poly ADP-ribose polymerase) enzymes. By inhibiting these enzymes, PARP inhibitors prevent cancer cells from repairing their damaged DNA, leading to genomic instability and cell death. This makes PARP inhibitors particularly effective against cancers that are driven by mutations in the BRCA genes, such as breast, ovarian, and prostate cancers.
Side effects of PARP inhibitors (PARPi)
Side effects of PARPi depend on the individual and whether other treatments are used in conjunction with this treatment, such as hormone therapy and radiation therapy. Some common side effects may include:
Low red blood cell count
Nausea
Fatigue
Less common side effects include:
Decreased bone or muscle mass
Dizziness
Changes in taste perception
Current Health Canada-approved PARP inhibitors (PARPi) for prostate cancer
Olaparib (Lynparza): approved for metastatic castration-resistant prostate cancer (mCRPC)
Niraparib (Akeega) and abiraterone acetate tablets, plus prednisone or prednisolone: approved for BRCA+ metastatic castration-resistant prostate cancer (mCRPC)
Currently, in most provinces in Canada, people with mCRPC and BRCA (or ATM gene) mutations qualify for PARP inhibitor treatment, so this is one reason that it is important to test for genetic background: to understand cancer and access all the available treatments. In addition, if a mutation is found, family members may become eligible for testing for the inherited gene so that they have the opportunity to prevent their own cancers in the future.
Summary
While hormone therapy and chemotherapy are often effective for castration-sensitive prostate cancer, new therapies are needed to improve survival in patients with castration-resistant prostate cancer (CRPC).
PARP inhibitors are a type of targeted therapy drug that has been shown to be very effective against certain prostate cancers, especially those with BRCA mutations, and greatly improve the survival of mCRPC patients.
Additional Reading
The landscape of cancer treatment is constantly evolving, and recent pre-clinical and clinical research provides a growing rationale for combining PARP inhibitors like olaparib with hormone therapies, like abiraterone and enzalutamide (N. Agarwal et al. / European Journal of Cancer 192 (2023) 113249)
This section reviews two recent studies that investigate Olaparib’s standalone efficiency, efficiency in combination with standard hormone therapy (NHAs), and impact on patients with BRCA mutations. This section is recommended for readers seeking a more in-depth understanding of the subject.
Olaparib’s Standalone Efficiency:
In the PROfound study, olaparib treatment alone was tested as a treatment for HRR Mutation Positive Metastatic Castration-Resistant Prostate Cancer. It compared olaparib 300 mg twice daily (2 x 150 mg tablets) monotherapy against the standard treatment of new hormonal agents (a type of hormone treatment; NHAs) in patients. The significance of the PROfound study lies in its design – a randomized, open-label, multicentre, phase III trial involving 387 participants.
In the PROfound study, HRR-mutated patients (n = 256) taking olaparib showed significant improvements in reducing progression and enhancing overall survival compared to patients (n = 130) who received the standard treatment, which are NHAs. However, it's important to note a slight increase in the number of patients discontinuing olaparib compared to the standard of care due to treatment-related adverse events, with common reasons including low blood counts. This contrast highlights the balance between treatment efficacy and patient tolerance. (PM reference; version 20OCT2024)
Olaparib in Combination Therapy:
In another clinical study, PROpel, the efficacy of olaparib was further put to the test, this time in combination with the NHAs abiraterone and prednisone/prednisolone, for treating patients with BRCA-mutated metastatic castration-resistant prostate cancer (mCRPC).
In the PROpel study, which randomized 796 patients (399 olaparib/abiraterone: 397 placebo/abiraterone), offers critical insights. Particularly for the subgroup of patients with BRCA mutations, the study demonstrated clinically meaningful responses, including a reduced rate of radiological progression and better overall survival. Similar to the PROfound study, patients on the therapy typically experienced side effects related to reduced blood counts, fatigue, and nausea. (PM reference; version 20OCT2024)
Understanding these findings is key for shaping new treatment recommendations and offering new hope in the battle against cancer. With growing research recognizing the potential of combination therapy in treating prostate cancer, they have the potential to improve patient care and provide more effective and personalized treatment options.
References
1. Prostate Cancer stats: https://www.canada.ca/en/public-health/services/publications/diseases-conditions/prostate-cancer.html
2. CCS Prostate cancer common therapies: https://cancer.ca/en/cancer-information/cancer-types/prostate/treatment
3. NCI prostate cancer therapies: https://www.cancer.gov/about-cancer/treatment/types/hormone-therapy
4. John Hopkins U Medicine types of therapies: https://www.hopkinsmedicine.org/health/conditions-and-diseases/prostate-cancer/immunotherapy-for-prostate-cancer
5. Synthetic lethality: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5528309/
6. Harvard guys: https://genesdev.cshlp.org/content/early/2021/08/11/gad.348479.121
7. Side effects: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7292736/
8. XRAY list of approved PARP inhibitors: https://www.facingourrisk.org/info/risk-management-and-treatment/cancer-treatment/by-cancer-type/prostate/targeted-and-immunotherapy
9. The FDA approved talazoparib study: https://doi.org/10.1016/S0140-6736(23)01055-3
10. The Drug and Health Product Register: https://hpr-rps.hres.ca/reg-content/summary-basis-decision-result.php?lang=en